Staphylococcus aureus under microscope 100x – Staphylococcus aureus, a ubiquitous bacterium, unveils its intricate world under the microscope at 100x magnification, revealing a wealth of fascinating characteristics that underpin its clinical significance. This article delves into the microscopic realm of S. aureus, exploring its morphology, virulence mechanisms, and diagnostic implications.
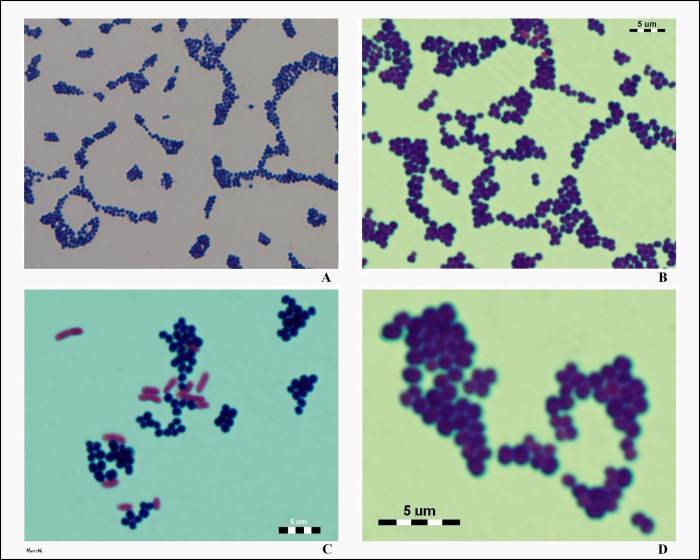
The Gram-stained image of S. aureus reveals its distinctive Gram-positive nature, characterized by a thick peptidoglycan layer that retains the crystal violet dye. The bacteria typically appear as spherical or slightly oval-shaped cocci, arranged in grape-like clusters. Their compact arrangement and relatively small size (0.5-1.5
μm) contribute to their ability to colonize and invade host tissues.
Gram Stain Appearance
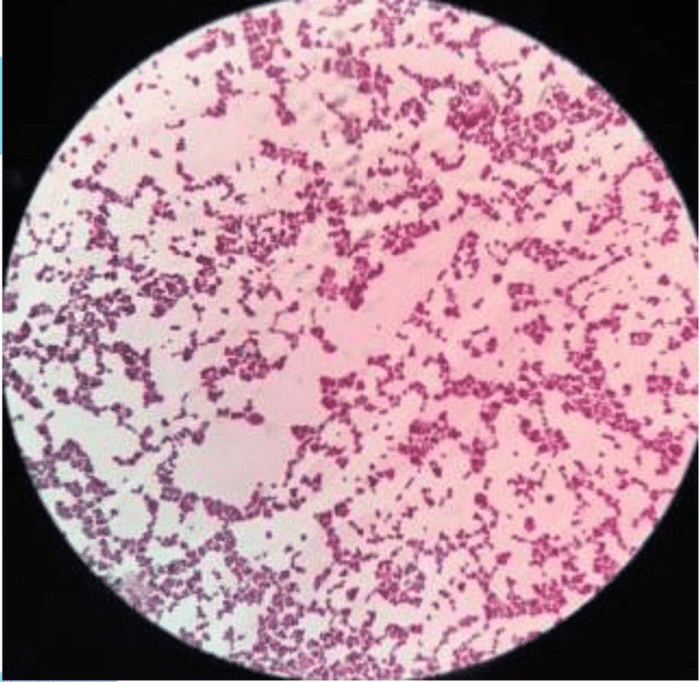
Under a microscope using Gram staining, Staphylococcus aureusappears as Gram-positive bacteria. Gram staining is a laboratory technique used to differentiate bacteria based on their cell wall structure. Gram-positive bacteria have a thick peptidoglycan layer in their cell walls, which retains the Gram stain, resulting in a purple color.
Staphylococcus aureusis typically spherical or coccus-shaped, with a diameter of approximately 0.5-1.5 micrometers. The bacteria often occur in clusters or pairs, giving them a “grape-like” appearance. The Gram-stained image below shows Staphylococcus aureusas purple-colored cocci arranged in clusters.

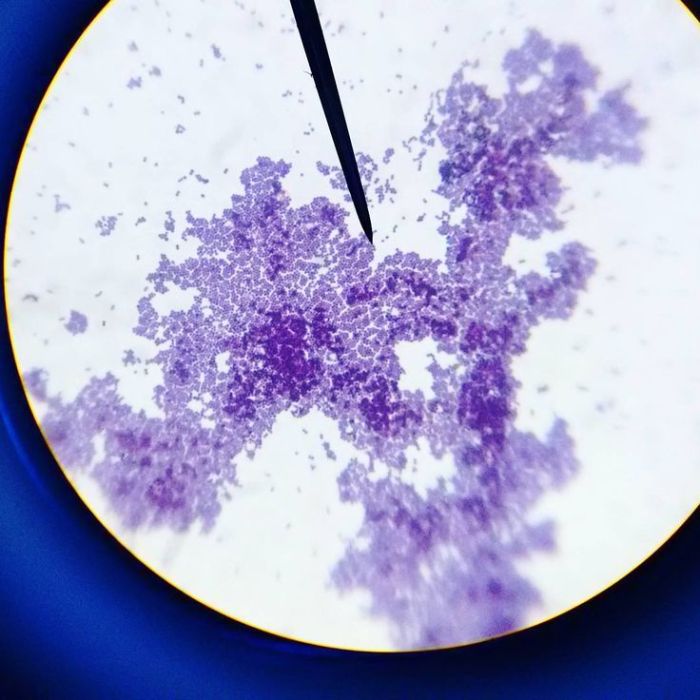
Colony Morphology
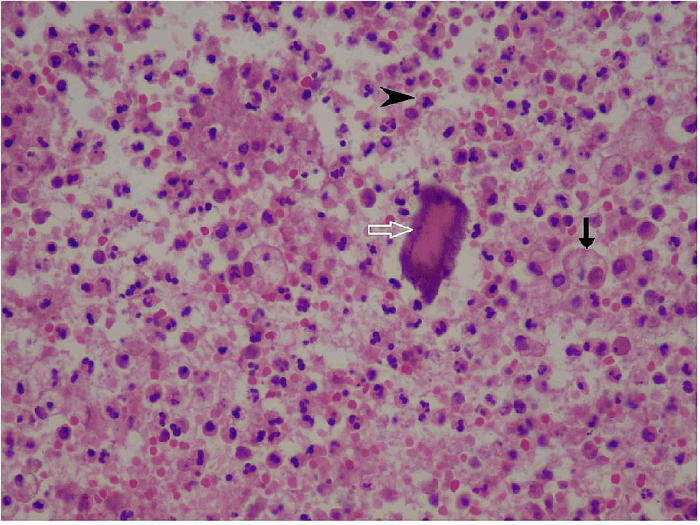
On different growth media, Staphylococcus aureusexhibits distinct colony characteristics. On blood agar, the colonies are typically round, convex, and golden-yellow in color. The colonies may have a beta-hemolytic zone around them, indicating the production of hemolysins, which are enzymes that break down red blood cells.
On nutrient agar, the colonies are usually white to cream-colored and opaque. They have a smooth, buttery texture and may produce a characteristic grape-like odor.

Pathogenicity and Virulence Factors
Staphylococcus aureusis a highly pathogenic bacterium that possesses a wide range of virulence factors. These factors contribute to its ability to cause a variety of infections, including skin and soft tissue infections, respiratory infections, and bloodstream infections.
Some of the major virulence factors of Staphylococcus aureusinclude:
| Virulence Factor | Function |
|---|---|
| Coagulase | Converts fibrinogen into fibrin, forming a protective fibrin clot around the bacteria |
| Protein A | Binds to the Fc portion of antibodies, interfering with the host’s immune response |
| Hemolysins | Lyse red blood cells, releasing nutrients for the bacteria |
| Exotoxins | Damage host cells and tissues, causing inflammation and tissue destruction |
Clinical Significance
Staphylococcus aureusis a major human pathogen, causing a wide range of infections. The most common infections include:
- Skin and soft tissue infections: boils, abscesses, cellulitis, impetigo
- Respiratory infections: pneumonia, bronchitis, sinusitis
- Bloodstream infections: sepsis, endocarditis
- Toxic shock syndrome
- Osteomyelitis
The symptoms of Staphylococcus aureusinfections can vary depending on the site of infection. However, common symptoms include pain, swelling, redness, fever, and chills.
Diagnostic Methods
Staphylococcus aureuscan be identified using a variety of laboratory methods. These methods include:
- Culture: Staphylococcus aureuscan be grown on blood agar or nutrient agar plates. The colonies can be identified by their characteristic appearance and hemolytic properties.
- Biochemical tests: Staphylococcus aureuscan be identified using a variety of biochemical tests, such as the catalase test, coagulase test, and DNase test.
- Molecular techniques: Molecular techniques, such as PCR, can be used to identify Staphylococcus aureusby detecting specific DNA sequences.
| Diagnostic Method | Sensitivity | Specificity |
|---|---|---|
| Culture | High | High |
| Biochemical tests | Moderate | High |
| Molecular techniques | High | High |
Treatment and Prevention: Staphylococcus Aureus Under Microscope 100x
The treatment of Staphylococcus aureusinfections depends on the severity of the infection and the susceptibility of the bacteria to antibiotics. In most cases, antibiotic therapy is the primary treatment for Staphylococcus aureusinfections.
Commonly used antibiotics include:
- Penicillinase-resistant penicillins (e.g., methicillin, oxacillin)
- Cephalosporins (e.g., cefazolin, cefuroxime)
- Glycopeptides (e.g., vancomycin, teicoplanin)
- Linezolid
- Clindamycin
In addition to antibiotic therapy, surgical drainage or debridement may be necessary in some cases.
Preventing the spread of Staphylococcus aureusis important. Good hygiene practices, such as handwashing and covering open wounds, can help prevent the spread of the bacteria.
Question Bank
What is the typical size and shape of Staphylococcus aureus under a microscope?
S. aureus appears as spherical or slightly oval-shaped cocci, typically ranging in size from 0.5 to 1.5 μm.
Why is the Gram stain important for identifying Staphylococcus aureus?
The Gram stain differentiates between Gram-positive and Gram-negative bacteria based on their cell wall structure. S. aureus is Gram-positive, retaining the crystal violet dye due to its thick peptidoglycan layer.
What are the key virulence factors of Staphylococcus aureus?
S. aureus possesses an array of virulence factors, including toxins (e.g., alpha-toxin, toxic shock syndrome toxin), enzymes (e.g., coagulase, nuclease), and surface proteins (e.g., protein A, fibronectin-binding proteins) that contribute to its pathogenicity.